Get Tech Tips
Subscribe to free tech tips.
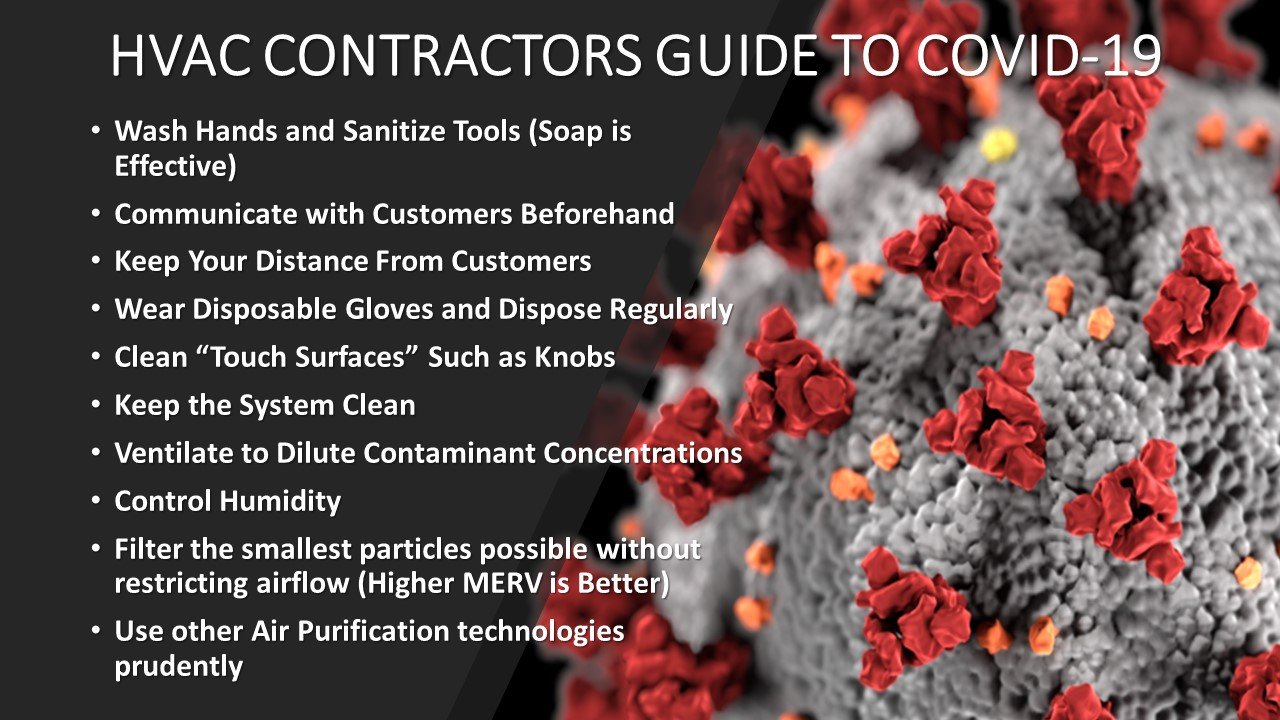
HVAC Contractors Guide to COVID-19 (SARS-CoV-2, Coronavirus)
UPDATED VERSION AS OF 4/1/2020
As HVAC contractors, we are tasked with keeping staff and customers safe during the outbreak, and we are relied upon to provide some guidance to customers about how to protect themselves against the virus in the air.
For employers and employees looking to navigate the new FMLA/FFRCA legislation, we put together a document covering the main points, and we included the federal poster on the topic HERE.
At HVAC School, we've been doing a lot of reading and listening to people with a lot more knowledge on these topics than we had before writing this guide. Even after conducting all the best research possible, it must be said we are not microbiologists, epidemiologists, or industrial hygienists. Our understanding of this outbreak is ever-evolving, and we will update this guide as new information becomes available. Still, the best resource for general information regarding prevention and care is available at the CDC website.
Other important industry resources:
ASHRAE COVID-19 (CORONAVIRUS) PREPAREDNESS RESOURCES
EPA Biological Pollutants' Impact on Indoor Air Quality
EPA Green Cleaning and Sanitizing Guide
Latest COVID 19 projections in the US and by State

Virus Basics
As with many things in our trade, it is helpful to gain a simple mental picture of how things work, even if it isn't a perfect representation.
The virus isn't “alive” in the way that fungus or bacteria is alive. It is a spiky sphere that contains genetic information (in the case of SARS-CoV-2, it is all RNA) that causes the host cells to “make” more of the virus.
When we ingest or inhale the SARS-CoV-2 virus, it attaches itself to our cells and “injects” that genetic information into our cells, causing them to create more of the virus to infect more cells with new spiky spheres. Some of these get expelled from our mouths and noses when we cough, sneeze, or talk. Some emissions make their way onto our hands when we touch things.
The key thing to get our heads around:
The virus spreads outside of us, but it only REPLICATES inside of us.
We are the virus factories; our own cells make it based on the tiny plans planted in them. This matters because if we think of viruses like bacteria or fungi that are living and growing, then we will come to incorrect conclusions.
Viruses have a fatty (lipid) coating that makes up the sphere, and the spikes that make it stick are little proteins.
When the fatty layer of protection is broken, the genetic information inside the virus can no longer get into your cells, rendering it non-infectious. In fact, when we say that something “kills” a virus, that is what we are really saying because it wasn't alive to start with.
One big factor in infection is the immune function of the person who gets the virus. If someone has immunity, it means that their immune system has identified the virus as a risk due to current or previous experience, and the body sends antibodies to surround and neutralize the virus.
A vaccine is generally a weakened or deactivated version of a virus. Vaccines are injected into a person so their immune system can “learn” to fight the virus before an actual infection occurs.
As professionals who interface with consumer health, it must be our mission to help provide an indoor atmosphere that promotes immune function AND protects against contaminants.
That means we must seek not only to neutralize viruses but look to contribute to all the factors that can create and maintain a healthier indoor environment. This includes:
- Good air ventilation and circulation to reduce airborne chemicals (VOCs) and CO2
- Humidity control
- Temperature control
- Air filtration
- Carbon monoxide monitoring and testing to keep it as close to zero as we can
- Control over duct and building envelope leakage to keep control over indoor air factors and quality
This webinar video from Nate Adams and Retrotec is an excellent source of detailed information and is one of the resources I used heavily in writing this.
Use Soap/Detergents
The reason soap works well to deactivate the virus is the nature of the bonds that form on the fatty lipid shell of the virus. The soap breaks the lipid shell apart when hands are washed with enough time and friction. The “antibacterial” properties of some soaps are just that, antibacterial, which means they work against bacteria, not viruses.

The difference between a soap and a detergent is that soap is natural and made from animal and plant sources, and detergents are synthetic products generally specifically designed to overcome some technical challenges with soaps.
A molecular biologist I spoke to summed it up this way:
“Basically, if it makes suds, it's doing what you need.”
Obviously, the effectiveness of any cleaning process depends on many things like the amount of soap used, dwell time, and friction.

This isn't to say that using an anti-viral disinfectant AFTER cleaning is a bad idea. Some surfaces can be tough to clean with soap reliably, and disinfectants can also disrupt and deactivate the viral membrane. Make sure to use an EPA-LISTED DISINFECTANT that is also specifically listed and labeled for HVAC use.

There is evidence that high-temperature steam is also effective as a sanitizer. This is a quote from the EPA Green Cleaning and Disinfection Guide:
“Dry vapor steam cleaners have been shown to be very effective for disinfecting and is approved for food contact surfaces as well as other surfaces.”
As always, we strike a balance between safety and effectiveness, and we look to use effective and safe products when neutralizing viruses. We need to consider the technician and the occupants in our decision-making.

How Do We “Catch” (become infected with) a Virus?
There are several different ways that a virus is transmitted, but the Coronavirus (SARS-CoV-2) is transmitted primarily in two ways:
- Bio-aerosols: Basically viruses contained in our saliva that come from our coughs, sneezes, and breath, which appear to make up the majority of the risk.
- Surface contamination: Occurs when someone gets viruses on their hands and then touches a surface; then someone else comes along and touches that same surface. Surfaces can also become contaminated when bio-aerosols fall and settle on surfaces.
The virus survives best inside our bodies, and once it leaves, the clock starts ticking for how long it survives before it becomes deactivated and non-infectious.
Again, the virus doesn't “grow” outside of us, it just spreads out, and some other unlucky person can either breathe it in or pick it up from surfaces and then transfer it to their face from their hands.
This is why hand-washing, disposable gloves (regularly changed), and masks are effective at preventing the spread. In the USA, we have not widely used respirator masks such as the N95, primarily because they are cumbersome and uncomfortable to wear all the time and, most of all, because there is a shortage of them for healthcare workers.
Wearing surgical masks may not effectively protect the wearer but can assist in containing the bio-aerosols in the mask, preventing others from being infected by the wearer. This is somewhat disputed by well-researched sources, like this one, with the conclusion being that almost any mask is better than no mask.
Either way, we know that quality masks like N95 are the best bet, but we need to save them for healthcare workers at this time.
If you are using masks, there is a lot of discussion about how to sanitize them without disposing of them when there is a short supply. This research cited by Stanford seems to show that 30-min in a 156°F oven is one of the better options.

HOWEVER, the report is careful to state that there are many factors to sanitize masks, and they STRONGLY ADVISE AGAINST sanitizing at home in a home oven.
Health care workers are at a much higher risk of contracting the virus due to procedures such as intubation, which is why respirators are a necessity for them and not necessarily for other workers outside of healthcare, like HVAC techs.
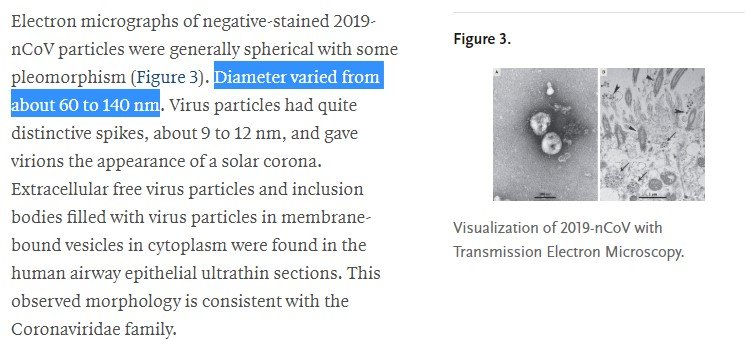
Viruses are small—much smaller than dust, pollen, dander, bacteria, and fungus. That means they may remain suspended in the air given the right conditions and are hard to catch in typical air filters. But it isn't as bleak as it may seem.
This article from Smart Air covers why many high MERV filters can still help significantly with viruses, even if the “holes” in the filter are larger than the size of the virus.
Obviously, HEPA filtration is still the gold standard for capturing tiny particles, but even HEPA captures really tiny particles via a phenomenon called diffusion.
There are many papers and a lot of back-and-forth on how long the virus can survive in the air and on various surfaces. The answer is that there is still a lot we don't know, but we do know that it can survive in the air, but it appears unlikely that an infectious dose will travel all the way into the HVAC equipment and survive long enough to be a risk to HVAC professionals. That doesn't mean we shouldn't take precautions, such as wearing gloves, bagging filters, and even wearing masks while removing filters. Nevertheless, risks do appear to be low, even in worst-case scenarios like medical HVAC applications.

We know for sure the virus lasts longer on stainless steel and plastic than it does on copper. So, is it time to go back to copper doorknobs and handrails?
Our greatest risk by far… is still when we are around people who carry the virus.
So, to summarize some virus basics:
- Viruses aren't alive in the same way as bacteria and fungus.
- People carry the virus, and it replicates INSIDE the body; it does not grow or reproduce on surfaces.
- Viruses are tiny and hard to catch when compared to most other particulates.
- Soap and detergent cleaners work well on viruses.
- Sanitizing with appropriately tested and rated sanitizers is still a good idea.
- Good masks do help, but medical professionals need them most.
Protecting Workers and Customers
For an HVAC contractor, it is in our best interest as an “essential service provider” to keep our technicians and customers safe while still doing our jobs. The following is a list of policies and procedures you could put into place to help.
Standard Practices
- Wash hands thoroughly for 20 seconds with soap and water using vigorous friction, including:
- Before eating
- After each call
- After bathroom breaks
- After fueling vehicle
- Employees should stay home if they show any symptoms; make it easy for them to stay home.
- Check temperature every morning before the start of work, and stay home if it exceeds 100.4°F.
- Practice social distancing of 6’ – no shaking hands.
- Don’t touch the face.
- Sanitize tools, steering wheel, and cell phone with 70/30 isopropyl alcohol or other approved sanitizer (don't mix products).
- Avoid ride-alongs when possible.
Customer Interaction Zones
- Ask customers if any occupants have symptoms before dispatching. If so, limit to only necessary calls, wear a respirator in the customer interaction zones (when available), and request the customer to wear a surgical mask.
- Request all customers to pre-open doors for the technician (where possible) to limit surface contact and maintain 6’ of distance.
- Wear disposable gloves and safety glasses while in the customer work area when handling knobs and surfaces in the customer zone (N95 masks once there is no longer a shortage).
- Wear work-appropriate gloves while performing work tasks.
- Sanitize knobs and other common touch areas at the end of the work.
Servicing Equipment
- When servicing equipment, use the usual PPE of gloves, safety glasses, or goggles as appropriate for the task and standard PPE masks/respirators when changing filters or working with chemicals.
- Service filters and evaporators with the blower off.
- Use only approved cleaning and disinfection products, and follow the specific directions for use on HVAC equipment, including coils, blowers, and air filters.
- Washing then sanitizing evaporator coils, blower wheels, and cabinets with approved cleaners and processes is always a good idea anyway.
Remember, the greatest risk of infection is when you are in proximity to other people, not in the equipment itself.
Improving Customer Outcomes
Another thing our customers look to us for is ways to help protect themselves and their families from infection. Along the way, we need to make sure we:
- Do no harm
- Tell the truth
- Provide solutions that represent a value
- Execute the solutions properly
This is surprisingly hard in the case of this virus because it isn't living, and it propagates inside people, not on surfaces or in equipment.
Factors
- More indoor time by occupants means more indoor pollution and exposure.
- Maintaining healthy indoor conditions improves immune and respiratory function (annualreviews.org, erswhitebook.org, epa.gov).
- More surface sanitizing means more chemical use indoors and more ventilation and dilution needs.
- Filtration is required for particles such as dander, dust mites, and pollen. Dilution is required for VOCs and CO2.
- CO monitoring is a must for buildings with any fuel-burning appliances due to the impacts on pulmonary function of even low levels of CO.
Ventilation
There are many different ways to bring in outdoor air. As we ventilate, we need to filter and control the humidity of that air if it is too humid, too dry, or full of particulate matter. It helps to dilute indoor contaminants with outdoor air so long as we:
- Provide filtered, humidity-controlled outdoor air according to ASHRAE 62.2 or similar (dehumidification or humidification may prove challenging at high ventilation rates).
- Ventilate during occupancy or according to CO2/VOC levels.
- CO2 levels higher than 1000 PPM are attributed to decreased cognitive function and perception.
 I love this guidance for a simple way to filter room air on a low budget from the Hayward Score.
I love this guidance for a simple way to filter room air on a low budget from the Hayward Score.

Filtration
- HEPA filtration where possible
- MERV 13+ is ideal with 4” or thicker media
- Activated carbon/charcoal filters can help to reduce VOCs and O3
- Filter outdoor air independently/redundantly
- Ensure system static pressures are within design
- Counteract higher resistance air filtration with a greater surface area to reduce filter pressure drops
Humidity Control
- Humidity that is too low may make COVID-19 worse
- Humidity control between 30-60% at all times is highly recommended, with 30% being ideal for winter in cold/dry climates, and 50-55% is ideal for summer in warm/humid climates
- Humidity control also impacts VOC off-gassing, bacteria, fungus, and O3
Kaleb Saleeby wrote an excellent overview of these three factors HERE.
Be Prudent Regarding IAQ Products
There are numerous IAQ products on the market with varying levels of effectiveness and safety. At HVAC School, we advocate for more independent testing under real-world conditions, testing against a wide range of particles, VOCs, and biological contaminants. We also advocate for peer-reviewed studies of these independent tests. As it stands, products like direct air filtration are well established, whereas products that use active production of oxidizers have not been as well tested in a truly independent fashion.
Because of this, I suggest only selling IAQ products where:
- You understand the underlying technology, not just the marketing or trade name.
- You have sought out the best independent studies you can find.
- You have a grasp on all of the risks (all products have risks).
- You ensure the products are installed properly.
- The customer has been communicated with based on science and real research.
- You can monitor the IAQ characteristics with a quality monitor BEFORE and AFTER.
Avoid falling for:
- The idea that any core IAQ technology on the market is proprietary
- Claims of kill rates or capture rates without the specific test criteria
- Claims that things are “NASA technology” or “space-approved,” etc., without understanding what that means
Risks to Watch For
Every IAQ product has some risk factors, even if they are minor. For example, putting in a better air filter (from a MERV standpoint) can restrict airflow, bringing in more outdoor air could increase or decrease humidity beyond the safe range, etc.
Even some of our favorite IAQ solutions can cause problems if we don't plan for them and think them through. Here are some common things to watch for in common “boxed” purification solutions:
- Products that produce O3
- UV
- UV has been shown effective in irradiating metal surfaces in close proximity (doi.org)
- Any UV light that shines on a surface that is not metal where VOCs can be produced
- UV lights and eyesight
- Oxidizing air purification
- Incomplete degradation
- Impacts of ions directly on respiratory function
- Efficacy in large areas/high-velocity air streams
The following are some great videos to watch to understand more about these topics:
(Employees) What to do if you are sick:
- Follow the CDC Guidelines.
- Stay Home! Stay Home! Stay Home!
- Call your healthcare provider or visit an online clinic. Follow their instructions.
- Do not go to the doctor (clinic, urgent care, or ER) if your symptoms are mild.
- Call 911 if your symptoms are life-threatening.
(Managers and Owners) What to do right now:
- Follow CDC’s guidelines to create an “Infectious Disease Outbreak Response Plan” for your place of business.
- Do employees all know who to contact if they’re sick?
- Who will do the cleaning procedure?
- Who is responsible for the risk assessment?
- Who decides if the business will shut down? And open back up? How will you notify everyone?
- Do you need to notify customers?
(Managers and Owners) What to do in your place of business if an employee is sick or “presumed COVID-19 positive:”
- Follow CDC’s instructions for “Disinfecting Your Facility if Someone is Sick.”
- General information (as of 21-Mar-2020): Most places in the US are not able to test everyone who has the symptoms of COVID-19. Therefore, it is most likely that if an employee becomes sick with COVID-19 symptoms, you will not have test results to confirm if they are positive or negative. Most likely, they will be evaluated, and if their symptoms are close, they will be given instructions to act as if they are COVID-19 positive. They will be “presumed COVID-19 positive.”
(Managers and Owners) What to do if an employee has had contact with or lives with someone who is sick or “presumed COVID-19 positive:”
- Follow CDC’s Risk Assessment procedure for “Management of Persons with Potential Coronavirus Disease 2019 (COVID-19) Exposures.”
- One section says:
Contacts of Asymptomatic People Exposed to COVID-19: CDC does not recommend testing, symptom monitoring, or special management for people exposed to asymptomatic people with potential exposures to SARS-CoV-2 (i.e. in a household). People who have been exposed to “contacts of contacts” are not considered exposed to SARS-CoV-2.
In closing, this guide is written to help contractors and technicians work more safely and keep customers safe. It is not the final word on any of these topics and SHOULD NOT be used without FIRST reading current CDC and OSHA guidelines, as well as consulting an experienced industrial hygienist.
—Bryan
Some More Excellent Resources
Healthy Indoors Magazine COVID Webinar Series
Find out more about the health of your home environment with the Hayward Score

 I love this guidance for a simple way to filter room air on a low budget from the
I love this guidance for a simple way to filter room air on a low budget from the 






Comments
To leave a comment, you need to log in.
Log In